Introduction:
Bringing a new life into the world is an incredible journey, but it’s also a time of profound transformation for both the mother and the newborn. The postpartum period, often referred to as the “fourth trimester,” is a crucial phase that deserves as much attention and preparation as pregnancy itself. During this time, your body and mind are recovering from the birthing process, and your focus naturally shifts to the well-being of your precious bundle of joy.
To navigate this beautiful yet challenging chapter of motherhood, it’s essential to have a well-organized plan in place. That’s where our comprehensive postpartum checklist comes into play. Whether you’re a first-time mom or a seasoned pro, this guide is designed to help you prepare for every aspect of postpartum care, ensuring that both you and your baby get the best possible start on your journey together.
Why a Postpartum Checklist Matters:
You may be wondering why you need a checklist at all. After all, parenthood is about going with the flow and adapting, right? While flexibility is undoubtedly essential, a well-thought-out postpartum checklist serves several vital purposes:
- Peace of Mind: Knowing that you have all the necessary items and information at your fingertips can reduce stress and anxiety, allowing you to focus on bonding with your newborn.
- Efficiency: Parenthood can be demanding, and time can become a precious commodity. A checklist ensures that you’re not running back and forth to gather forgotten essentials in the middle of the night.
- Support: Sharing your checklist with friends and family can help them understand your needs better and offer practical assistance during this transitional period.
- Self-Care: The postpartum checklist isn’t just about baby supplies; it also includes items for your own recovery and self-care. Taking care of yourself is crucial to being the best parent you can be.
Throughout this blog post, we’ll walk you through every stage of the postpartum journey. From packing your hospital bag to creating a self-care routine, recognizing postpartum depression symptoms to planning postpartum visits and assessments, we’ve got you covered. Whether you’re a mom who just gave birth, planning for a C-section, or looking for ways to support your postpartum doula, this guide will provide you with valuable insights and practical tips.
So, let’s embark on this journey together. Grab your favorite notebook or your smartphone, because you’re going to want to take notes. Our aim is to empower you with knowledge, inspire you to embrace self-care, and ensure that your postpartum experience is as joyful and rewarding as possible. Let’s get started on building your ultimate postpartum checklist!
Download this blog post: Postpartum Checklist: Essentials for Mom and Baby as a FREE PDF Here.
Section 2: Hospital Bag Checklist
As your due date approaches, one of the most important tasks on your pre-baby to-do list is packing your hospital bag. It’s a momentous event that can be both exciting and a bit nerve-wracking, especially for first-time moms. The key to a smooth hospital stay and postpartum recovery is preparation, and that starts with a well-thought-out hospital bag checklist.
Subsection 2.1: Postpartum Essentials for Mom
Your hospital bag should be divided into two main sections: one for you and one for your baby. In this subsection, we’ll focus on the essentials you’ll need to ensure your comfort and well-being during your hospital stay.
- Comfortable Clothing: Pack loose-fitting, comfortable clothing for your stay. Think soft pajamas, cozy robes, and comfortable underwear. You’ll want to be at ease as you recover.
- Toiletries: Don’t forget your toothbrush, toothpaste, shampoo, conditioner, soap, and any other personal hygiene items you use daily. Hospitals may provide some basics, but having your own can make you feel more comfortable.
- Nursing Bras and Pads: If you plan to breastfeed, nursing bras and breast pads are essential. They provide support and help manage leaks.
- Maxi Pads: You’ll experience postpartum bleeding (lochia) after birth. Make sure to pack a supply of heavy-duty maxi pads.
- Slippers and Non-Slip Socks: Hospitals can be chilly, and you’ll want something cozy for your feet.
- Comfort Items: Bring items that bring you comfort, such as a favorite pillow, blanket, or stuffed animal. Familiar items can help create a more soothing environment.
- Snacks: Hospital food may not always satisfy your cravings. Packing some of your favorite snacks can be a real treat during your stay.
- Entertainment: Bring a book, magazines, or a tablet with headphones to pass the time while resting.
- Important Documents: Don’t forget your ID, insurance information, and any necessary hospital paperwork. Having these ready can streamline the admission process.
Subsection 2.2: Baby’s Needs
Now let’s focus on what your baby will need during your hospital stay and for the journey home.
- Baby Clothes: Pack a few outfits for your baby, including onesies, sleepers, and a going-home outfit. Remember that newborns can be messy, so having extra outfits is a good idea.
- Diapers and Wipes: Hospitals usually provide initial diapers and wipes, but it’s a good idea to have some extras on hand, especially for the trip home.
- Swaddle Blankets: Swaddle blankets can help keep your baby snug and comfortable. They also make for adorable photo opportunities.
- Car Seat: Your baby will need a car seat for the journey home. Ensure it’s properly installed and ready to go.
- Feeding Supplies: If you’re breastfeeding, bring your breast pump, nursing pillow, and any other necessary supplies. If you’re using formula, pack formula, bottles, and sterilizing equipment.
- Baby Essentials Bag: Consider packing a small bag with baby essentials like pacifiers, baby lotion, and a baby nail clipper. These items can come in handy.
Remember that your hospital stay may vary in duration, so it’s better to overprepare than to be caught without something you need. Plus, having your essentials ready will allow you to focus on your recovery and bonding with your baby.
In the next section, we’ll delve into specific considerations for moms who have had a C-section, so stay tuned for that. For now, get that hospital bag ready, and let’s ensure you’re fully prepared for your postpartum journey.
Section 3: C-Section Postpartum Checklist
For some expectant mothers, the birth plan may include a cesarean section (C-section) delivery. While the procedure has become increasingly common and safe, it does require some specific considerations during the postpartum period. In this section, we’ll provide a comprehensive C-section postpartum checklist to ensure a smooth and comfortable recovery.
Subsection 3.1: Recovery Essentials
- Abdominal Support Belt: Consider investing in an abdominal support belt or binder. This can provide added support to your incision site and alleviate discomfort.
- Pain Medication: Discuss pain management options with your healthcare provider. You may need prescription pain medication or over-the-counter pain relievers to manage discomfort.
- Incision Care: Follow your healthcare provider’s instructions for incision care. Keep the incision clean and dry, and watch for signs of infection.
- Limited Lifting: Avoid heavy lifting or strenuous activities in the weeks following your C-section. This includes lifting older children or heavy objects.
- Comfortable Clothing: Choose loose-fitting, breathable clothing that won’t irritate your incision site.
Subsection 3.2: Breastfeeding Considerations
- Nursing Positions: Experiment with different nursing positions to find one that minimizes pressure on your incision.
- Nursing Pillow: A nursing pillow can provide support and comfort during breastfeeding sessions.
Subsection 3.3: Emotional Support
- Emotional Well-Being: Understand that recovering from a C-section can be emotionally challenging. Seek emotional support from loved ones or consider joining a postpartum support group.
- Body Image: Be patient with your body’s healing process. It’s natural for your abdomen to feel different after a C-section, and it may take time to regain strength and tone.
Subsection 3.4: Rest and Self-Care
- Rest and Sleep: Rest is crucial for recovery. Accept help from family and friends, and prioritize sleep whenever possible.
- Gentle Movement: While you should avoid strenuous activities, gentle walking can aid in circulation and promote healing.
- Hydration and Nutrition: Stay hydrated and nourished to support your body’s recovery. High-fiber foods can help prevent constipation, a common concern after surgery.
- Self-Care Routine: Incorporate self-care activities into your daily routine. Whether it’s a warm bath, meditation, or simply reading a book, take time for yourself.
Subsection 3.5: Follow-Up Appointments
- Scheduled Check-Ups: Attend all scheduled postoperative follow-up appointments with your healthcare provider. They will monitor your incision healing and overall recovery.
- Discuss Future Birth Plans: Use this time to discuss any concerns or questions you have about future pregnancies and birth plans with your healthcare provider.
Remember that recovery after a C-section is unique to each individual. It’s important to listen to your body and follow your healthcare provider’s guidance closely. With proper care and support, you can have a successful and healthy postpartum period following a C-section.
In the next section, we’ll delve into postpartum care at home, providing a comprehensive checklist to help you navigate the weeks and months following childbirth. Stay tuned for more practical guidance on your postpartum journey.
Section 4: Postpartum Care at Home
Once you’ve welcomed your baby into the world and completed your hospital stay, it’s time to transition to postpartum care at home. This section of our ultimate postpartum checklist will guide you through the essential steps to ensure your comfort and well-being during this crucial phase of your post-birth journey.
Subsection 4.1: Physical Recovery
- Pain Management: Continue to take any prescribed pain medication as directed by your healthcare provider. Over-the-counter options may also be recommended.
- Incision Care: Maintain proper care of your C-section incision or perineal area. Keep it clean, dry, and watch for any signs of infection.
- Perineal Care: For vaginal births, consider warm sitz baths to soothe the perineal area. Over-the-counter pain relief sprays or creams may provide relief as well.
- Pelvic Floor Exercises: Begin gentle pelvic floor exercises to aid in recovery and regain muscle strength.
- Hydration and Nutrition: Continue to prioritize a balanced diet and stay well-hydrated. Adequate nutrition is vital for healing and energy.
- Rest and Sleep: Aim for as much rest as possible during the early weeks. Nap when your baby naps to combat sleep deprivation.
Subsection 4.2: Emotional Well-Being
- Baby Blues vs. PPD: Be aware of your emotional well-being. While the baby blues are common and temporary, postpartum depression (PPD) requires professional support. Seek help if you experience persistent feelings of sadness, anxiety, or hopelessness.
- Talk About Your Feelings: Share your thoughts and feelings with a trusted friend or family member. Sometimes, simply talking about your experiences can provide emotional relief.
Subsection 4.3: Breastfeeding and Infant Care
- Latch and Feeding: Continue to work on breastfeeding techniques and seek support from lactation consultants if needed. Ensure your baby is latching correctly and feeding well.
- Baby’s Sleep Schedule: Understand that newborns have irregular sleep patterns. Create a soothing bedtime routine to help your baby differentiate between day and night.
- Diaper Changes: Keep track of your baby’s diaper changes, as this can provide insight into their feeding and hydration.
Subsection 4.4: Support System
- Accept Help: Don’t hesitate to accept offers of help from friends and family. Whether it’s assistance with household chores or someone to watch the baby while you rest, support can make a significant difference.
- Support Groups: Consider joining postpartum support groups or online communities. Connecting with other new parents can provide a sense of camaraderie and valuable advice.
Subsection 4.5: Birth Control and Future Planning
- Birth Control: Discuss birth control options with your healthcare provider. Postpartum contraception is an essential consideration for family planning.
- Future Family Planning: If you’re thinking about future pregnancies, discuss your plans with your healthcare provider. They can provide guidance on timing and preparations.
Remember that the postpartum period is a time of adjustment and learning for both you and your baby. Be patient with yourself and allow time for recovery. Seek help and support when needed, and focus on nurturing the precious bond between you and your newborn.
In the next section, we’ll delve into the importance of recognizing postpartum depression symptoms and seeking help when necessary. Understanding and addressing this critical issue is vital for the well-being of both mom and baby.
Download this blog post as a FREE PDF here – Postpartum Checklist: Essentials for Mom and Baby
Section 5: Recognizing Postpartum Depression (PPD) Symptoms
The postpartum period, often associated with joy and the arrival of a new life, can also bring emotional challenges, including postpartum depression (PPD). Understanding the signs and symptoms of PPD is crucial for both new moms and their support networks. In this section, we’ll delve into what PPD is, how to recognize its symptoms, and why seeking help is paramount.
Subsection 5.1: Understanding Postpartum Depression (PPD)
- What Is PPD?: Postpartum depression is a type of clinical depression that affects some women after childbirth. It’s not a sign of weakness or a character flaw; it’s a medical condition that requires attention.
- Prevalence: PPD is more common than you might think. It can affect up to 1 in 7 new mothers.
Subsection 5.2: Recognizing PPD Symptoms
- Persistent Sadness: Feeling intensely sad, empty, or hopeless for most of the day, nearly every day.
- Loss of Interest: Losing interest in activities that were once enjoyable.
- Fatigue: Overwhelming fatigue, even with adequate rest.
- Changes in Appetite: Significant changes in appetite and weight, either loss or gain.
- Sleep Disturbances: Difficulty falling asleep or staying asleep, unrelated to your baby’s sleep patterns.
- Irritability and Anxiety: Feeling unusually irritable, anxious, or on edge.
- Difficulty Concentrating: Struggling to focus, make decisions, or remember things.
- Feelings of Guilt or Worthlessness: Persistent feelings of guilt, worthlessness, or inadequacy as a mother.
- Withdrawal from Loved Ones: Isolating yourself from friends and family.
- Physical Symptoms: Experiencing physical symptoms like headaches or digestive issues.
- Thoughts of Self-Harm or Harm to the Baby: In severe cases, experiencing thoughts of self-harm or harm to the baby. These are emergency situations requiring immediate attention.
Subsection 5.3: Seeking Help for PPD
- Don’t Suffer in Silence: If you suspect you may have PPD, reach out for help. Speak to your healthcare provider, a therapist, or a counselor. Remember that PPD is treatable, and seeking help is a sign of strength.
- Support System: Lean on your support system, including friends and family, to help you through this challenging time. They can provide emotional support and assistance with daily tasks.
- Medication and Therapy: Your healthcare provider may recommend medication, therapy, or a combination of both to treat PPD. These treatments can be highly effective.
- Postpartum Support Groups: Consider joining postpartum support groups, either in person or online. Connecting with others who have experienced PPD can provide valuable insights and reduce feelings of isolation.
- Communicate with Your Partner: If you have a partner, open and honest communication is key. Share your feelings and concerns with them so they can offer support.
Remember, PPD is not your fault, and it doesn’t mean you’re a bad parent. It’s a medical condition that requires attention and treatment. By recognizing the symptoms and seeking help early, you can take the first steps toward recovery and a happier, healthier postpartum experience for both you and your baby.
In the next section, we’ll discuss the importance of having a postpartum plan and incorporating self-care into your routine, which can be essential for emotional well-being during the postpartum period.
Section 6: Postpartum Plan and Self-Care Checklist
Creating a postpartum plan and prioritizing self-care are essential components of a smooth and emotionally healthy postpartum journey. In this section, we’ll explore why having a postpartum plan matters and provide a comprehensive self-care checklist to help you navigate this transformative phase of motherhood.
Subsection 6.1: The Importance of a Postpartum Plan
- What Is a Postpartum Plan?: A postpartum plan is a roadmap for your first few weeks or months after childbirth. It outlines your expectations, support network, and self-care strategies.
- Why Have a Postpartum Plan?: Having a plan in place helps reduce stress and provides a sense of control during a time of significant change. It ensures you prioritize self-care and emotional well-being.
Subsection 6.2: Creating Your Postpartum Plan
- Set Realistic Expectations: Understand that the postpartum period is a time of adjustment. Be kind to yourself and acknowledge that it’s okay to ask for help.
- Identify Your Support Network: Make a list of friends, family members, or professionals who can provide support. Share your plan with them and let them know how they can assist you.
- Prioritize Rest: Plan for restful periods throughout the day. Enlist someone’s help to care for the baby while you nap or simply take a break.
- Meal Planning: Prepare or arrange for easy-to-make meals or meal deliveries. Proper nutrition is crucial for postpartum recovery.
- Set Boundaries: Be clear about your boundaries with visitors and well-wishers. Don’t hesitate to let them know when it’s a good time to visit or if you need some space.
- Self-Care Activities: Include self-care activities in your daily routine. Whether it’s a warm bath, meditation, journaling, or a short walk, make time for yourself.
Subsection 6.3: Self-Care Checklist
- Hydration: Drink plenty of water throughout the day to stay well-hydrated.
- Nutrition: Eat a balanced diet that nourishes your body and supports healing.
- Rest: Prioritize sleep and rest whenever you can. Sleep deprivation can impact your emotional well-being.
- Physical Activity: Incorporate gentle physical activity into your routine once your healthcare provider gives the green light.
- Connect with Others: Maintain social connections through phone calls, video chats, or in-person visits when comfortable.
- Support Groups: Consider joining postpartum support groups to connect with other mothers experiencing similar challenges.
- Delegate Tasks: Don’t hesitate to delegate household tasks to friends or family members. Allow them to help with chores, grocery shopping, or childcare.
- Express Your Feelings: Talk openly with a trusted friend, family member, or therapist about your emotions and experiences.
- Limit Screen Time: Reduce excessive exposure to social media, as it can contribute to feelings of inadequacy.
- Celebrate Small Achievements: Acknowledge and celebrate your daily accomplishments, no matter how small they may seem.
Remember that self-care is not selfish; it’s essential for your well-being and your ability to care for your baby. A well-planned postpartum journey that includes self-care will not only benefit you but also create a positive environment for your newborn.
In the following section, we’ll discuss the importance of postpartum visits and assessments, which play a vital role in monitoring your health and the health of your baby as you transition into motherhood.
Section 7: Postpartum Visits and Assessments
Postpartum care involves not only self-care but also regular check-ins with healthcare providers to ensure both you and your baby are healthy and thriving. In this section, we’ll delve into the importance of postpartum visits and assessments, what to expect during these appointments, and how they contribute to a smooth postpartum journey.
Subsection 7.1: The Importance of Postpartum Visits
- Monitoring Health: Postpartum visits allow healthcare providers to monitor your physical and emotional well-being. They ensure any potential issues are identified and addressed promptly.
- Baby’s Health: These visits are also essential for monitoring your baby’s growth and development, ensuring they are meeting milestones and thriving.
- Support and Guidance: Postpartum visits provide an opportunity to discuss any concerns, receive guidance on infant care, and seek support for postpartum issues.
Subsection 7.2: Postpartum Visit Schedule
- First Week: Your first postpartum visit typically occurs within the first week after birth, often around day 3-5. This visit may take place at home or in a clinic and focuses on assessing both mother and baby’s well-being.
- 6 Weeks Postpartum: The six-week postpartum visit is a crucial milestone. It allows your healthcare provider to evaluate your physical recovery and assess any potential complications. You’ll also discuss birth control options during this appointment.
- Additional Visits: Depending on your specific needs and circumstances, you may have additional postpartum visits. These may be recommended for mothers who experienced complications during birth or have pre-existing medical conditions.
Subsection 7.3: What to Expect During Postpartum Visits
- Physical Assessment: Your healthcare provider will conduct a physical examination, checking your incision site (if you had a C-section), abdominal muscles, and pelvic floor.
- Mental Health Evaluation: Discuss your emotional well-being during these visits. It’s essential to be honest about any feelings of sadness, anxiety, or other emotional challenges.
- Breastfeeding Support: If you’re breastfeeding, your provider can offer guidance on latch, positioning, and any breastfeeding concerns.
- Baby’s Growth: Your baby’s weight, length, and overall growth will be monitored to ensure they are thriving.
- Contraception Discussion: The six-week visit is an opportunity to discuss birth control options, especially if you wish to prevent future pregnancies.
- Questions and Concerns: Bring a list of any questions or concerns you have to your postpartum visits. Your healthcare provider is there to provide answers and support.
Subsection 7.4: Preparing for Postpartum Visits
- Documentation: Keep a record of your baby’s feeding habits, diaper changes, and any concerns you may have. This can help you and your healthcare provider track your baby’s progress.
- Medications: Bring a list of any medications or supplements you are taking, including prenatal vitamins or pain relievers.
- Support: Consider having a trusted friend or family member accompany you to your postpartum visits, especially if you have concerns about discussing emotional well-being.
- Prepare Questions: Write down any questions or topics you want to discuss during the visit to ensure you don’t forget important details.
Postpartum visits are a vital component of your postpartum care plan. They provide an opportunity for ongoing support, monitoring, and guidance during this transitional phase. Don’t hesitate to reach out to your healthcare provider between scheduled visits if you have any immediate concerns or questions.
In the next section, we’ll delve into the role of a postpartum doula and what you can expect during a postpartum doula visit, offering additional support during the early weeks of motherhood.
Section 8: Postpartum Doula Support
The postpartum period can be both exhilarating and overwhelming. As you adjust to your new role as a mother, having the support of a postpartum doula can make a significant difference. In this section, we’ll explore the role of a postpartum doula, the benefits they offer, and what you can expect during a postpartum doula visit.
Subsection 8.1: Who Is a Postpartum Doula?
- Definition: A postpartum doula is a trained and experienced professional who provides physical, emotional, and informational support to mothers and their families during the postpartum period.
- Non-Medical Support: Postpartum doulas do not provide medical care but focus on practical assistance and guidance to help new mothers transition into parenthood.
Subsection 8.2: The Benefits of Postpartum Doula Support
- Emotional Support: Postpartum doulas offer emotional support, a listening ear, and reassurance during a time of change and uncertainty.
- Infant Care Guidance: They can assist with infant care, including feeding support, soothing techniques, and baby care basics.
- Breastfeeding Support: For breastfeeding mothers, doulas provide guidance on latching, positioning, and addressing common breastfeeding challenges.
- Household Assistance: Postpartum doulas can help with light household chores, meal preparation, and sibling care, allowing you to focus on recovery and bonding with your baby.
- Self-Care: They encourage and facilitate self-care, ensuring that you prioritize your well-being during the postpartum period.
Subsection 8.3: What to Expect During a Postpartum Doula Visit
- Assessment: At the beginning of each visit, your postpartum doula will assess how you and your baby are doing. They will ask about your needs and any specific concerns.
- Supportive Presence: Your doula will provide a calming presence, offering emotional support and reassurance.
- Feeding Support: If you’re breastfeeding, your doula can assist with latch and positioning, helping you and your baby have a successful feeding session.
- Infant Care: They may offer tips and guidance on infant care, including diapering, swaddling, and soothing techniques.
- Self-Care Planning: Your doula will help you plan self-care activities, ensuring you take time for yourself.
- Household Assistance: If needed, your doula can assist with light household chores, meal preparation, or caring for older siblings.
- Answering Questions: Feel free to ask any questions or share your concerns with your doula. They are there to provide information and guidance.
Subsection 8.4: How to Find a Postpartum Doula
- Research: Start by researching postpartum doulas in your area. You can often find them through online directories or recommendations from other mothers.
- Interview: Schedule interviews with potential doulas to discuss your needs, expectations, and their approach to postpartum support.
- References: Ask for references or reviews from previous clients to ensure the doula is a good fit for your family.
- Certification: Consider working with a certified postpartum doula who has completed training and adheres to a code of ethics.
Having a postpartum doula can be a valuable addition to your support network during the postpartum period. They offer practical assistance, emotional support, and expert guidance to help you navigate the early weeks of motherhood with confidence.
In the following section, we’ll discuss postnatal assessments and the importance of postpartum care kit checklist to ensure your health and well-being after childbirth.
Download this blog post as a FREE PDF here – Postpartum Checklist: Essentials for Mom and Baby
Section 9: Postnatal Assessments and the Postpartum Care Kit Checklist
After childbirth, both you and your baby require ongoing care and monitoring. Postnatal assessments for the mother and having a well-prepared postpartum care kit can help ensure a smooth recovery and a healthy start for your baby. In this section, we’ll explore why these assessments matter and provide a detailed checklist for your postpartum care kit.
Subsection 9.1: The Importance of Postnatal Assessments
- Mother’s Health: Postnatal assessments for mothers are crucial to monitor physical recovery, especially after a C-section or a complicated birth.
- Baby’s Well-Being: For your baby, postnatal assessments help ensure they are thriving and meeting developmental milestones.
- Early Detection: Assessments can detect any potential complications or health issues early, allowing for prompt intervention.
Subsection 9.2: Mother’s Postnatal Assessment
- Incision Check: If you had a C-section, your healthcare provider will assess your incision for signs of infection, proper healing, and any potential complications.
- Physical Examination: A general physical examination will be conducted to check for any postpartum complications or issues.
- Emotional Well-Being: Your mental health and emotional well-being will be discussed. Be open and honest about any feelings of sadness, anxiety, or other emotional challenges.
Subsection 9.3: Baby’s Postnatal Assessment
- Weight and Measurements: Your baby’s weight, length, and head circumference will be measured to track growth.
- Feeding Assessment: Your healthcare provider will assess your baby’s feeding habits and ensure they are latching and feeding well.
- Developmental Milestones: Your provider will check if your baby is meeting developmental milestones appropriate for their age.
Subsection 9.4: The Postpartum Care Kit Checklist
- Postpartum Pads: Stock up on heavy-duty maxi pads to manage postpartum bleeding.
- Perineal Spray or Cream: To soothe discomfort in the perineal area after vaginal birth.
- Sitz Bath: A sitz bath can help relieve discomfort and promote healing.
- Pain Medication: Over-the-counter pain relievers or any prescribed medications for pain management.
- Nursing Supplies: Nursing bras, breast pads, and nipple cream if you plan to breastfeed.
- Hydration and Nutrition: Easy-to-grab snacks and a reusable water bottle to stay hydrated.
- Stool Softeners: To ease any discomfort during bowel movements.
- Comfortable Clothing: Loose-fitting, comfortable clothing and supportive underwear.
- Baby Essentials: Diapers, wipes, swaddle blankets, baby clothes, and a baby thermometer.
- Baby Feeding Supplies: If formula feeding, bottles, formula, and sterilizing equipment.
- Baby Care Products: Baby lotion, baby nail clippers, and a baby hairbrush.
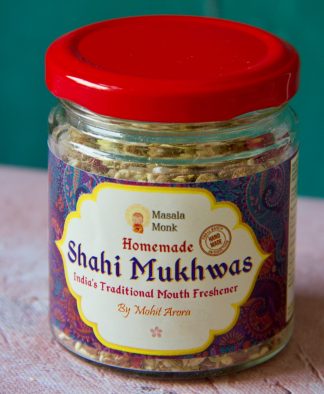
- Self-Care Items: Items like a journal, a soothing scented candle, or your favorite book for moments of relaxation.
- Medications: If you’re on any medications, ensure you have a sufficient supply.
- Important Documents: Keep important documents, such as your ID and insurance information, handy.
- Phone Charger: Don’t forget your phone charger for staying connected and capturing those precious moments.
Having a well-prepared postpartum care kit checklist ensures that you have all the essentials you’ll need during your recovery and for caring for your newborn. Make sure your kit is ready well in advance of your due date.
In the next section, we’ll discuss postpartum discharge and provide guidance on what to expect as you transition from the hospital to home, ensuring a seamless start to your postpartum journey.
Section 10: Postpartum Discharge and Transition to Home
The time has come to leave the hospital and start your postpartum journey at home. This transition can be exciting but also filled with questions and adjustments. In this section, we’ll explore what to expect during postpartum discharge, how to prepare for your journey home, and tips for a seamless transition.
Subsection 10.1: What to Expect During Postpartum Discharge
- Timing: Postpartum discharge typically occurs 24-48 hours after a vaginal birth and 72-96 hours after a C-section. However, this timeline may vary depending on individual circumstances.
- Baby’s Health: Your baby will undergo a final check-up to ensure they are healthy and ready for discharge. This includes weight, feeding, and overall well-being assessments.
- Mother’s Health: You will receive instructions and guidance on postpartum care, including incision care (if applicable), pain management, and any medications you may need.
- Paperwork: Be prepared to complete any necessary paperwork, including your baby’s birth certificate and any hospital-related documents.
Subsection 10.2: Preparing for the Transition Home
- Travel Arrangements: Ensure you have a safe and comfortable mode of transportation for both you and your baby. Install a car seat that meets safety standards.
- Postpartum Care Kit: Double-check that your postpartum care kit is packed and ready to go. Having essential supplies on hand can reduce stress during the transition.
- Support Person: Arrange for someone to accompany you and help with transportation, especially if you had a C-section or expect to be less mobile.
- Baby Essentials: Make sure you have all the necessary baby supplies, including diapers, wipes, clothing, and a properly installed car seat.
- Home Preparation: Ensure your home is ready for your return. This may include setting up a comfortable nursing or feeding station and having necessary items within easy reach.
Subsection 10.3: Tips for a Smooth Transition
- Ask Questions: Don’t hesitate to ask your healthcare provider any last-minute questions or concerns before leaving the hospital.
- Feeding Plan: If you’re breastfeeding or formula-feeding, have a feeding plan in place. Know when and how your baby will be fed.
- Take It Slow: Be patient with yourself and your baby as you adjust to the new environment. Transitioning home can be overwhelming, so take it one step at a time.
- Accept Help: Allow friends and family to assist you with household tasks or caring for your baby. Accepting help can make the transition smoother.
- Sleep When Possible: Prioritize rest whenever you can. Sleep deprivation is common with a newborn, so take advantage of moments to nap.
- Emotional Well-Being: Continue to monitor your emotional well-being. Talk to your support system about your feelings and seek help if needed.
- Follow Postpartum Care Instructions: Adhere to the postpartum care instructions provided by your healthcare provider, including any medications or incision care.
- Postpartum Visits: Make sure you have scheduled postpartum visits with your healthcare provider to monitor your recovery and your baby’s health.
Transitioning from the hospital to home can be a joyful but challenging experience. Being well-prepared and having a support system in place can help ease the transition and allow you to focus on bonding with your baby and your own recovery.
In the final section of this comprehensive postpartum checklist, we’ll offer some closing thoughts and remind you of the importance of self-care and seeking support during your postpartum journey.
Section 11: Closing Thoughts and the Importance of Self-Care
Congratulations on embarking on your postpartum journey! As you prepare to embrace motherhood, it’s crucial to remember that taking care of yourself is equally as important as caring for your baby. In this final section, we’ll provide some closing thoughts and highlight the importance of self-care and seeking support during this transformative period.
Subsection 11.1: The Postpartum Journey
- A Time of Transformation: The postpartum period is a time of profound transformation. Your body, your family, and your daily routines are all adjusting to the presence of your new little one.
- Embrace the Journey: Embrace the changes and challenges that come with motherhood. It’s okay to feel overwhelmed or uncertain at times; these feelings are entirely normal.
Subsection 11.2: The Role of Self-Care
- Prioritize Yourself: Remember that self-care is not a luxury; it’s a necessity. Taking care of yourself physically and emotionally is vital for your well-being and your ability to care for your baby.
- Small Moments Matter: Self-care doesn’t have to be elaborate. Even taking a few minutes for yourself, whether it’s a quiet cup of tea or a short walk, can make a difference.
- Accept Help: Don’t be afraid to ask for and accept help from loved ones. They want to support you during this special time.
Subsection 11.3: Seeking Support
- Lean on Your Support System: Your friends and family are there to offer guidance, lend a listening ear, and provide assistance when needed.
- Join Support Groups: Consider joining postpartum support groups or online communities where you can connect with other new mothers facing similar challenges.
- Professional Support: If you’re struggling with postpartum depression, anxiety, or other mental health concerns, seek professional help. Therapy and counseling can provide valuable support and treatment.
- Postpartum Visits: Attend your postpartum visits with your healthcare provider to monitor your physical and emotional well-being.
Subsection 11.4: A Reminder for New Mothers
- You Are Enough: Remember that you are enough just as you are. You don’t have to be a perfect mother; your love and care are what truly matter.
- Celebrate Small Victories: Celebrate each small victory and milestone, both for yourself and your baby.
- Every Journey Is Unique: Your postpartum journey is unique to you. Don’t compare yourself to others or feel pressured to meet unrealistic standards.
As you embark on this new chapter of your life, know that you are surrounded by love and support. Cherish the moments with your baby, and be kind and patient with yourself. The postpartum period is a time of growth, learning, and incredible love.
In closing, we hope this comprehensive postpartum checklist has been a valuable resource for you as you prepare for your postpartum journey. Remember to prioritize self-care, seek support when needed, and savor the precious moments with your newborn. Wishing you a happy and healthy postpartum experience!
Download this blog post as a FREE PDF here – Postpartum Checklist: Essentials for Mom and Baby
FAQs:
- What is postpartum care, and why is it important?
- Postpartum care is the medical and emotional support provided to mothers after childbirth. It’s crucial for monitoring the mother’s physical and emotional well-being, as well as ensuring the health and development of the baby.
- When should I start preparing for postpartum care?
- It’s best to start preparing for postpartum care during your pregnancy, ideally in the second or third trimester. This allows you to have everything in place before your due date.
- What items should I include in my postpartum care kit?
- Your postpartum care kit should include items like postpartum pads, perineal spray or cream, pain medication, comfortable clothing, baby essentials, and self-care items. Refer to the checklist in the post for a detailed list.
- How can I recognize the symptoms of postpartum depression (PPD)?
- Symptoms of PPD include persistent sadness, loss of interest, fatigue, changes in appetite, irritability, difficulty concentrating, and thoughts of self-harm. Seek professional help if you experience these symptoms.
- What is the role of a postpartum doula, and when should I consider hiring one?
- A postpartum doula provides non-medical support, including emotional and practical assistance to new mothers. Consider hiring one if you need extra help with infant care, breastfeeding, or emotional support during the postpartum period.
- How often should I schedule postpartum visits with my healthcare provider?
- Typically, you should have a postpartum visit within the first week and another at around 6 weeks after childbirth. Additional visits may be scheduled based on your specific needs.
- What should I expect during postpartum discharge from the hospital?
- During postpartum discharge, your baby’s health will be assessed, and you’ll receive guidance on postpartum care and any necessary paperwork. It’s also an opportunity to ask any last-minute questions.
- How can I ensure a smooth transition from the hospital to home with my newborn?
- To ensure a smooth transition, arrange for safe transportation, have your postpartum care kit ready, prepare your home, and accept help from loved ones. Patience and self-care are key during this transition.
- What are some self-care tips for new mothers during the postpartum period?
- Self-care tips include prioritizing rest, accepting help, connecting with support systems, practicing small moments of self-care, and seeking professional help if needed.
- Is it normal to feel overwhelmed during the postpartum period?
- Yes, it’s entirely normal to feel overwhelmed during the postpartum period. It’s a time of adjustment and change. Reach out to your support system and healthcare provider if you need assistance.
Blog Tags: Postpartum care, Postpartum checklist, New mother, Postpartum depression, Postpartum doula, Postnatal assessment, Self-care, Postpartum discharge, Transition home, Newborn care