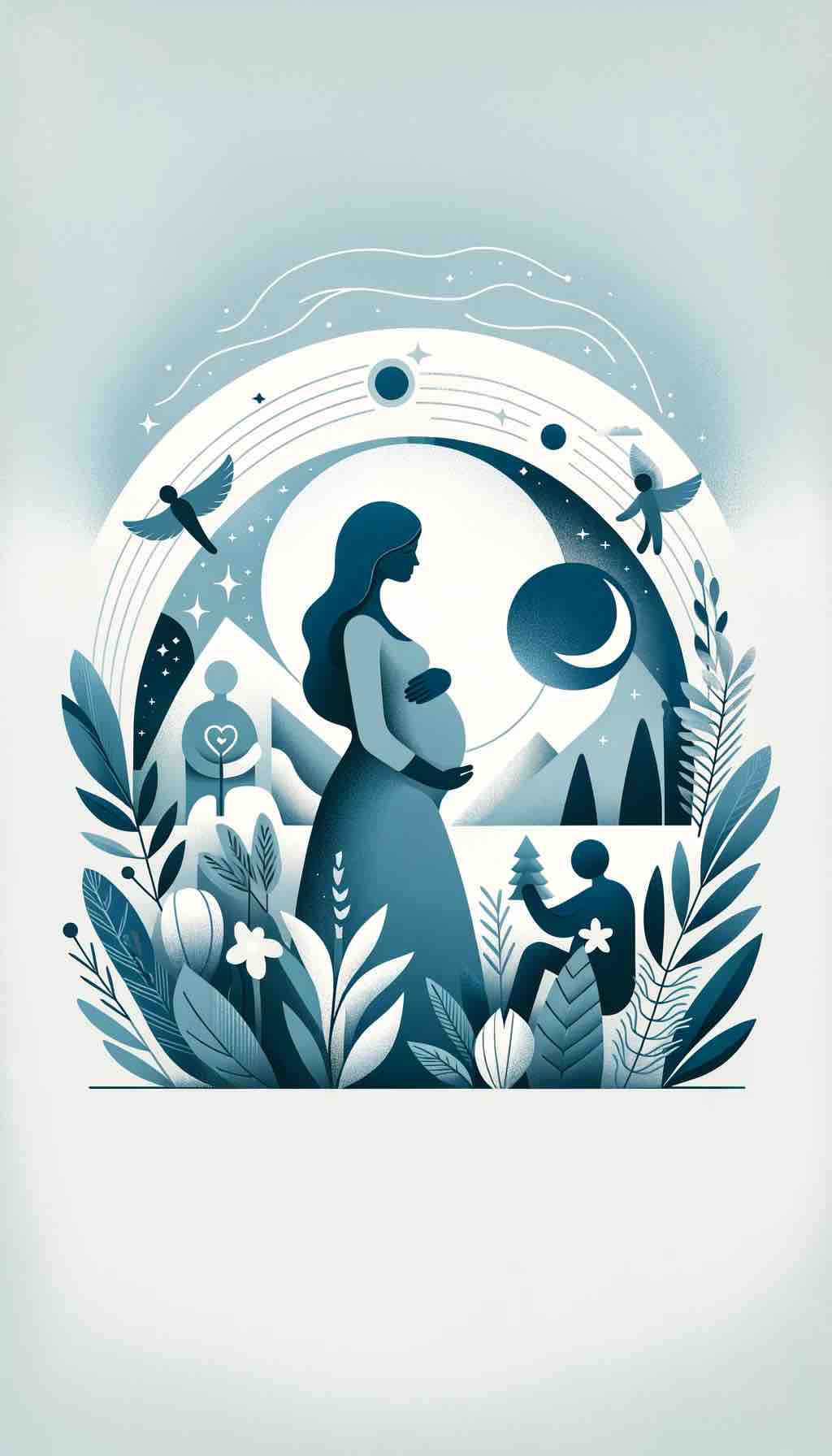
Have you ever found yourself standing in the middle of a room, wondering what you came in for, or forgetting simple words mid-conversation? These moments of mental fog, often chuckled about and dismissed as mere forgetfulness, are particularly familiar to expectant mothers. They call it the “pregnancy brain” – a term that encapsulates the cognitive shifts many women experience during pregnancy.
“Pregnancy brain” is more than an old wives’ tale; it’s a real phenomenon characterized by memory lapses, difficulty in concentrating, and occasional confusion. This cognitive haze is not just a quirky side effect of carrying a child; it’s a fascinating window into the profound changes a woman’s body and brain undergo during this critical phase of life. The term ‘pregnancy brain’ is not only endearing but also mystifying, reflecting the complex interplay of hormones, emotions, and neurological adaptations that occur during pregnancy.
From missed appointments to misplaced keys, these episodes of forgetfulness are often sources of amusement. But for those experiencing them, they can be a source of frustration and concern. What many don’t realize is that these changes are part of an intricate biological process. As the body nurtures a new life, it undergoes a remarkable transformation – and the brain is no exception.
So why does pregnancy brain happen? It’s a question that scientists and mothers alike have pondered. Research suggests that several factors contribute to these cognitive shifts. Hormonal changes, particularly the surge in estrogen and progesterone, play a significant role. These hormones, vital for the development of the fetus, also influence brain function, impacting memory and cognitive processing.
Furthermore, pregnancy is a time of significant emotional and physical change. The anticipation of a new family member, the planning and preparation for the arrival, and the physical demands of pregnancy can take a toll on mental faculties. Add to this the common sleep disturbances during pregnancy, and it’s no wonder that the brain might sometimes falter in its usual tasks.
But there’s more to pregnancy brain than forgetfulness and fog. Emerging research reveals that these cognitive changes may be part of an adaptive process, preparing the mother for bonding and responding to her baby’s needs. The brain, in its incredible capacity to adapt and evolve, might be fine-tuning its circuits, enhancing areas related to emotional regulation, empathy, and sensitivity – crucial skills for nurturing a newborn.
As we delve deeper into the intricacies of pregnancy brain, it’s essential to recognize and embrace these changes. They are not signs of a mind less capable, but rather indications of a brain remarkably adapting to one of life’s most profound journeys. In the coming sections, we’ll explore the scientific backing of pregnancy brain, unravel its causes, and provide practical tips for managing these cognitive changes. Stay tuned as we decode the mysteries of the maternal mind during pregnancy.
The Science of Pregnancy Brain: Navigating the Cognitive Seas of Motherhood
When we talk about the “pregnancy brain,” we often do so with a light-hearted chuckle. However, behind this humor lies a complex interplay of biological, neurological, and psychological changes that deserve a closer look. To understand this phenomenon, we must delve into the scientific underpinnings that govern the cognitive landscape of pregnancy.
A Deep Dive into Hormonal Highs and Lows
The most significant factor in pregnancy-related cognitive changes is the hormonal rollercoaster that women experience during this period. Pregnancy triggers a surge in hormones like estrogen and progesterone, which are crucial for the development of the fetus. However, these hormones also have a profound impact on brain chemistry. Estrogen, for instance, is known to play a vital role in cognitive functions, including memory and learning. Its increased levels during pregnancy can affect neurotransmitter systems and brain function, leading to the symptoms commonly associated with pregnancy brain.
Sleep Disruptions: A Key Culprit
Another critical factor contributing to pregnancy brain is sleep disruption. It’s no secret that expecting mothers often struggle with sleep, whether due to physical discomfort, anxiety, or hormonal changes. Poor sleep quality and reduced sleep duration can significantly impact cognitive functions. A lack of restful sleep leads to decreased alertness, impaired memory, and reduced cognitive abilities – all of which contribute to the foggy feeling of pregnancy brain.
Emotional Turbulence and Stress
Pregnancy is not just a physical journey but also an emotional one. The anticipation and anxiety about impending motherhood can contribute to cognitive changes. Stress, a common companion during pregnancy, can affect brain function, particularly in areas responsible for memory and decision-making. The brain’s preoccupation with the significant life transition of becoming a parent might redirect resources away from other cognitive tasks, leading to the forgetfulness and distraction commonly reported by pregnant women.
Brain Structure Changes: A Neurological Perspective
Recent studies have brought to light fascinating insights into how pregnancy can alter the brain’s structure. Research indicates that during pregnancy, women experience a reduction in gray matter in certain areas of the brain. Initially, this might sound alarming, but it’s actually an indication of the brain’s remarkable ability to adapt and prepare for motherhood. These changes, particularly in areas involved in processing social information and empathy, are believed to enhance a mother’s ability to bond with and respond to her infant. This synaptic pruning, a process similar to what occurs during adolescence, is the brain’s way of becoming more efficient and specialized.
Cognitive Changes: A Mixed Bag
The cognitive changes during pregnancy are not uniform and can vary significantly among women. While some might experience noticeable memory lapses and difficulty concentrating, others may observe minimal changes. It’s essential to understand that these variations are normal and reflect the unique ways in which different bodies adapt to pregnancy.
In summary, pregnancy brain is a multifaceted phenomenon, influenced by hormonal fluctuations, sleep patterns, emotional states, and neurological adaptations. It’s a testament to the remarkable resilience and adaptability of the human brain, particularly in response to the profound journey of bringing new life into the world. As we continue, we’ll explore the personal experiences of women navigating pregnancy brain, adding a layer of real-world context to these scientific findings.
Experiencing Pregnancy Brain: The Real-life Stories of Mothers-to-be
After exploring the scientific background of pregnancy brain, it’s time to bring this phenomenon down to the personal level. Every woman’s journey through pregnancy is unique, and understanding these individual experiences provides invaluable insights into the reality of cognitive changes during this transformative period.
Diverse Experiences: From Mild to Profound
The spectrum of pregnancy brain symptoms varies widely among women. For some, it manifests as minor forgetfulness – misplacing keys, forgetting appointments, or struggling to recall names. For others, the experience can be more profound, affecting their daily functioning and self-perception. This variability highlights the importance of approaching pregnancy brain as a highly individual experience, shaped by each woman’s unique physiological and psychological landscape.
Firsthand Accounts: The Voices of Expectant Mothers
To paint a true picture of pregnancy brain, let’s turn to the stories of those who have lived it. Many women describe moments of confusion and absent-mindedness that, while often humorous in retrospect, can be disconcerting when they occur. For example, a woman might recount the time she spent minutes searching for her phone while it was in her hand all along. Another might share her frustration over repeatedly forgetting why she walked into a room. These anecdotes not only offer a glimpse into the daily realities of pregnancy brain but also help in normalizing and validating these experiences.
Professional Perspectives: What the Experts Say
Medical professionals and psychologists emphasize that while pregnancy brain is a common experience, it’s not a sign of diminished intelligence or capability. They remind us that these cognitive shifts are temporary and typically resolve postpartum. Furthermore, experts encourage open conversations about these experiences, advocating for support and understanding from partners, family members, and healthcare providers. This professional reassurance is crucial in helping women navigate this period without undue stress or self-judgment.
The Role of Emotional and Mental Well-being
Emotional well-being plays a significant role in the experience of pregnancy brain. Feelings of overwhelm, anxiety about childbirth and parenthood, or concerns about balancing motherhood with other life responsibilities can exacerbate cognitive challenges. Recognizing and addressing these emotional factors is key to managing pregnancy brain symptoms. This might involve seeking support from a therapist, joining a support group, or simply having candid discussions with loved ones.
Cultural and Societal Influences
Cultural and societal attitudes towards pregnancy and motherhood also impact how women experience and perceive pregnancy brain. In cultures where pregnancy is highly valued and supported, women might feel more comfortable discussing and accepting these cognitive changes. Conversely, in societies where there is less understanding or acknowledgement of pregnancy brain, women might feel more isolated or stigmatized for experiencing these symptoms.
In conclusion, the personal experiences of pregnancy brain are as varied as they are enlightening. They provide a crucial human dimension to our understanding of this phenomenon, reminding us that behind every scientific explanation lies a tapestry of real-life stories. In the next section, we’ll delve into the causes behind pregnancy brain, exploring the various factors that contribute to this intriguing aspect of motherhood.
The Causes Behind Pregnancy Brain: Unraveling the Cognitive Puzzle
To understand the causes of pregnancy brain, we need to delve into a complex interplay of physiological, psychological, and environmental factors. Each of these elements plays a pivotal role in shaping the cognitive experiences of expectant mothers.
Hormonal Fluctuations: The Chemical Catalysts
One of the primary drivers of pregnancy brain is the dramatic shift in hormones experienced during pregnancy. Estrogen and progesterone levels soar, profoundly impacting the brain’s chemistry and function. These hormones influence neurotransmitter systems, which are crucial for cognition and mood regulation. Estrogen, for instance, is linked to memory formation and information processing. Its heightened levels during pregnancy can alter brain function in ways that manifest as forgetfulness or fuzzy thinking.
Sleep Disturbances: The Silent Disruptor
The quality and quantity of sleep significantly diminish during pregnancy, primarily due to physical discomfort and hormonal changes. Sleep is crucial for cognitive functions like memory consolidation and attention. Disrupted sleep patterns can therefore lead to impaired cognitive abilities, contributing to the symptoms of pregnancy brain. The link between sleep deprivation and reduced cognitive function is well-established, and for pregnant women, getting enough restful sleep can be a significant challenge.
Psychological Stress: The Mental Burden
Pregnancy is not just a physical but also an emotional journey, filled with anticipation, anxiety, and a myriad of concerns about the future. Psychological stress can take a toll on cognitive function. The mental load of preparing for a new baby, coupled with hormonal changes, can affect the brain’s ability to process information and recall details. Stress can also lead to distractibility and reduced concentration, further exacerbating the symptoms of pregnancy brain.
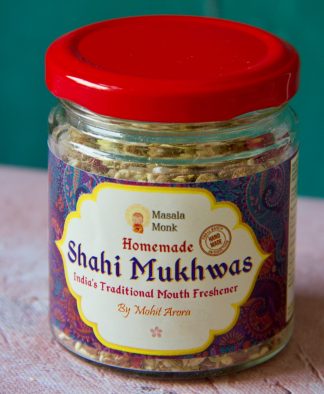
Nutritional Factors: The Role of Diet
Nutrition plays a critical role in brain health, and during pregnancy, the demand for certain nutrients increases. Deficiencies in essential nutrients like omega-3 fatty acids, iron, and vitamin D can impact cognitive function. A balanced diet, rich in brain-boosting nutrients, is therefore essential for maintaining cognitive health during pregnancy. Pregnant women need to ensure they are receiving adequate nutrition not just for the baby’s development but also for their own cognitive well-being.
Physical and Environmental Changes
The physical changes that accompany pregnancy, such as increased blood volume and changes in blood pressure, can also impact brain function. Moreover, environmental factors, including the level of support from family and society, work-related stress, and lifestyle changes, play a role in shaping the pregnancy brain experience. A supportive and understanding environment can help mitigate stress and improve overall cognitive well-being.
The Role of Adaptive Changes
Emerging research suggests that some aspects of pregnancy brain may be adaptive. The brain undergoes changes that enhance areas related to emotional regulation and empathy, potentially aiding in mother-infant bonding. These neurological adaptations might be the brain’s way of preparing the mother for the demands of caring for a newborn.
In summary, pregnancy brain is a multifaceted phenomenon, influenced by a confluence of hormonal, sleep-related, psychological, nutritional, and environmental factors. It’s a natural part of the pregnancy journey, reflecting the body’s incredible ability to adapt to the life-creating process. Understanding these causes helps demystify pregnancy brain and provides avenues for better management and support for expectant mothers. In the next section, we’ll explore practical strategies and tips for managing and embracing these cognitive changes during pregnancy.
Managing and Embracing Pregnancy Brain: Practical Strategies for Expectant Mothers
Now that we’ve explored the causes and experiences of pregnancy brain, it’s crucial to focus on how to manage and adapt to these cognitive changes. Expectant mothers can employ various strategies to cope with the challenges of pregnancy brain, turning a potentially frustrating experience into an opportunity for growth and adaptation.
1. Organizational Tools: Your New Best Friends
One of the most effective ways to combat forgetfulness is through organization. Utilizing tools like planners, calendars, and reminder apps can be a game-changer. They help in keeping track of appointments, to-do lists, and important dates. Digital tools are especially handy, as they often include customizable alerts and notifications. For those who prefer a more tactile approach, a traditional diary or planner can be equally beneficial.
2. Establishing Routines: The Power of Habit
Creating daily routines can greatly alleviate the mental load during pregnancy. Routines reduce the need to remember every small detail, as habitual actions become second nature. Simple routines, like always placing keys in the same spot or having a set bedtime ritual, can bring a sense of order and predictability, easing the cognitive burden.
3. Mindful Practices: Stress Reduction Techniques
Mindfulness and relaxation techniques can be particularly helpful in managing stress, a significant contributor to pregnancy brain. Practices such as meditation, prenatal yoga, or simple breathing exercises can help calm the mind, improve focus, and enhance memory retention. These techniques not only benefit cognitive function but also contribute to overall emotional well-being.
4. Nutritional Support: Brain-Boosting Diets
A balanced diet is crucial for cognitive health. Foods rich in omega-3 fatty acids, antioxidants, vitamins, and minerals support brain function. Incorporating foods like fatty fish, nuts, berries, and leafy greens can provide the necessary nutrients to bolster cognitive health. Staying hydrated is equally important, as dehydration can negatively impact concentration and memory.
5. Physical Activity: Keeping the Brain Sharp
Regular exercise is beneficial for both physical and mental health. Physical activity improves blood flow to the brain, enhancing cognitive functions and mood. Activities like walking, swimming, or prenatal exercise classes can be effective and enjoyable ways to stay active during pregnancy.
6. Adequate Rest: Prioritizing Sleep
Prioritizing sleep is essential for managing pregnancy brain. Good sleep hygiene, such as maintaining a consistent sleep schedule, creating a comfortable sleep environment, and avoiding caffeine and electronics before bedtime, can improve sleep quality. Naps can also be helpful in making up for lost nighttime sleep.
7. Social Support: The Role of Community
Having a supportive network can make a significant difference. Sharing experiences with other expectant mothers, either in person or through online communities, can provide emotional support and practical advice. Additionally, enlisting the help of family and friends for day-to-day tasks can alleviate stress and cognitive load.
8. Embracing the Change: A Positive Mindset
Finally, adopting a positive mindset towards pregnancy brain is crucial. Understanding that it’s a normal part of pregnancy can help in accepting and adapting to these changes. Celebrating the brain’s adaptability and focusing on the exciting journey of motherhood can transform the experience from one of frustration to one of empowerment.
In conclusion, while pregnancy brain can present challenges, there are numerous strategies to manage and even embrace these changes. By employing organizational tools, establishing routines, practicing mindfulness, maintaining a healthy diet and exercise regimen, prioritizing rest, seeking social support, and embracing a positive mindset, expectant mothers can navigate this unique period with confidence and grace. As we move forward, we will explore what to expect beyond pregnancy, including how long pregnancy brain lasts and its long-term implications.
Beyond Pregnancy: Understanding the Long-Term Impact of Pregnancy Brain
As we move beyond the immediate effects of pregnancy brain, it’s essential to consider its duration and any potential long-term implications. This understanding can provide reassurance to new mothers and those planning to extend their families.
Duration of Pregnancy Brain: A Temporary Phase
The experience of pregnancy brain is, for most women, a temporary condition. Typically, cognitive changes become more noticeable in the third trimester and can continue into the early postpartum period. However, the majority of women report a gradual return to their pre-pregnancy cognitive state within the first year after childbirth. This timeline can vary, with some mothers experiencing these changes for a shorter period and others for slightly longer.
Postpartum Period: A New Set of Cognitive Changes
The postpartum period brings its own set of cognitive and emotional challenges. New mothers may continue to experience some level of forgetfulness and mental fog, often exacerbated by sleep deprivation and the demands of caring for a newborn. However, these symptoms typically diminish as sleep patterns normalize and the new routines of motherhood are established.
The Role of Continued Hormonal Changes
Hormonal fluctuations continue to play a role in the cognitive experiences of new mothers. Postpartum hormonal adjustments can affect mood and memory, contributing to the continuation of pregnancy brain symptoms in the early postpartum period. As hormone levels gradually stabilize, so too does cognitive function.
Long-Term Cognitive Changes: What Research Suggests
Emerging research suggests that the brain changes experienced during pregnancy may have long-term effects, but these are not necessarily negative. Some studies indicate that the gray matter reductions in certain brain areas may lead to increased emotional regulation and empathy, potentially enhancing maternal responsiveness. These adaptations can be viewed as the brain’s long-term investment in parenthood.
The Importance of Mental and Physical Health
Maintaining mental and physical health remains crucial in the postpartum period. Practices that support cognitive function during pregnancy, such as a balanced diet, regular exercise, and sufficient sleep, continue to be important. Additionally, seeking support for postpartum mood disorders, should they arise, is vital for both cognitive health and overall well-being.
Supporting New Mothers: A Community Responsibility
The transition into motherhood is a significant life event, and the support of family, friends, and healthcare providers is essential. Understanding and acknowledging the cognitive changes new mothers may experience is an important aspect of this support. Creating a nurturing environment can help ease the transition and promote a healthy recovery from pregnancy brain.
In conclusion, while pregnancy brain is predominantly a temporary condition, its impact can extend into the early stages of motherhood. Understanding its duration and long-term implications can help women better prepare for and navigate this period. As research continues to shed light on these cognitive changes, we gain a deeper appreciation for the remarkable adaptability of the brain in response to the transformative experience of pregnancy and motherhood.
In the next section, we will wrap up our exploration of pregnancy brain, summarizing key points and offering final thoughts for expectant and new mothers navigating this unique journey.
Conclusion: Embracing the Journey of Pregnancy and Motherhood
As we conclude our exploration of pregnancy brain, it’s important to reflect on the key insights and takeaways from this fascinating phenomenon. Pregnancy brain, a blend of cognitive shifts, emotional changes, and physical adaptations, is not just a quirky side effect of pregnancy. It’s a testament to the incredible journey of creating and nurturing life.
Summarizing Pregnancy Brain
Pregnancy brain is a real and recognized condition characterized by forgetfulness, mental fog, and cognitive changes during pregnancy and sometimes extending into the postpartum period. Influenced by hormonal fluctuations, sleep disturbances, stress, and nutritional factors, these changes are a natural response to the physiological and emotional demands of pregnancy.
The Power of Adaptation
The human brain’s ability to adapt to pregnancy and motherhood is remarkable. Changes in brain structure, particularly in areas related to emotional regulation and empathy, suggest that pregnancy brain may be an evolutionary adaptation to enhance maternal bonding and responsiveness. This perspective not only demystifies pregnancy brain but also celebrates it as a sign of the brain’s incredible plasticity and resilience.
Practical Strategies for Management
We’ve discussed various strategies to manage the challenges of pregnancy brain, including organizational tools, establishing routines, mindfulness practices, maintaining a healthy diet, engaging in physical activity, prioritizing sleep, and seeking social support. These strategies are not only effective during pregnancy but are also beneficial practices for overall well-being.
The Role of Community and Support
The journey through pregnancy and into motherhood is deeply personal, yet it also thrives on community and support. Partners, family members, healthcare providers, and peers play a crucial role in providing understanding, assistance, and encouragement. Recognizing and validating the experiences of pregnancy brain contributes to a supportive environment that can significantly enhance the well-being of expectant and new mothers.
Looking Ahead
As research into pregnancy brain continues, we can expect to gain deeper insights into this complex phenomenon. Understanding the nuances of these cognitive changes can lead to better support systems, healthcare practices, and societal awareness, ultimately enriching the experience of motherhood.
In closing, pregnancy brain is more than a series of forgetful episodes; it’s a part of the profound transformation that encompasses pregnancy and motherhood. By embracing these changes with knowledge, preparation, and support, expectant and new mothers can navigate this journey with confidence and grace.
We hope this exploration of pregnancy brain has provided valuable insights and practical advice for those experiencing it and their loved ones. Remember, pregnancy and motherhood are journeys of both challenges and immense joy, and understanding the intricacies of pregnancy brain is a step towards embracing the full spectrum of this incredible life experience.
10 FAQs on Pregnancy Brain
- What is pregnancy brain?
- Pregnancy brain refers to the cognitive changes many women experience during pregnancy, characterized by forgetfulness, difficulty concentrating, and mental fog.
- Is pregnancy brain scientifically proven?
- Yes, research supports the existence of pregnancy brain, indicating hormonal changes, sleep disturbances, and psychological stress contribute to these cognitive shifts during pregnancy.
- How long does pregnancy brain last?
- Pregnancy brain typically peaks in the third trimester and can extend into the early postpartum period, with most women experiencing a return to their normal cognitive state within the first year after childbirth.
- Can pregnancy brain affect my work performance?
- It might. Pregnancy brain can lead to forgetfulness and reduced concentration, but many women effectively manage these symptoms with organizational strategies and lifestyle adjustments.
- Are there any long-term effects of pregnancy brain?
- Current research suggests that while pregnancy brain is mostly a temporary condition, the brain changes during pregnancy may enhance areas related to empathy and emotional regulation.
- What can I do to manage pregnancy brain?
- Employing organizational tools, establishing routines, practicing mindfulness, ensuring a healthy diet, staying physically active, and getting sufficient sleep are effective strategies.
- Does every pregnant woman experience pregnancy brain?
- Not necessarily. The intensity and presence of pregnancy brain symptoms vary among women.
- Can pregnancy brain lead to permanent memory loss?
- There’s no evidence to suggest that pregnancy brain leads to permanent memory loss. Most cognitive changes during pregnancy are temporary.
- Are there specific foods that can help with pregnancy brain?
- Foods rich in omega-3 fatty acids, antioxidants, vitamins, and minerals, such as fatty fish, nuts, berries, and leafy greens, can support brain health during pregnancy.
- Should I be worried about pregnancy brain?
- Pregnancy brain is a normal part of pregnancy for many women. It’s generally not a cause for concern, but if you experience significant cognitive changes or distress, consult with your healthcare provider.
Blog Tags for the Post
pregnancy, motherhood, cognitive changes, brain health, maternal wellness, hormonal impact, sleep and pregnancy, stress management, nutritional tips, postpartum care